Sleeve Gastrectomy
A new patient seeing Dr Phil Le Page for bariatric surgery will have a full assessment and discussion that allows you a good understanding of the types of weight loss surgery and which procedure is best for you. The Laparoscopic Sleeve Gastrectomy is the most common operation that Dr Le Page performs along with most bariatric surgeons in Australia and worldwide. There are good reasons why this operation is the most common. Dr Le Page will outline to you that the operation is a well-tolerated procedure and reliable procedure with its weight loss outcome. It also keeps a patient’s gastrointestinal system relatively unaltered thereby keeping things more simple for you. Despite this simplicity, it produces reliable profound weight loss that is very similar to the gastric bypass both in the short and long term. As with any surgery, there are rare risks present and it is important to understand these. Dr Le Page is very open and can explain this in understandable terms for you.
Preparing for Surgery and Recovery
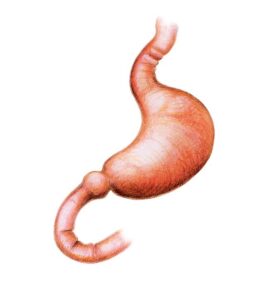
Following your initial consultation, you will be given information for your further education. Essentially, the stomach is the organ that receives the swallowed food and can stretch like a balloon. This is similar to blowing up a balloon at a kid’s party. This stretching ability is how we as humans can eat a whole dinner plate of food before feeling full. The effect of this reduction in the size of the stomach and turning it into a tube of a similar diameter to the rest of the bowel means that a patient experiences fullness and satiety very early after eating, early on even after a few mouthfuls.
You will also have an appointment with our dietitian. This will help you understand your diet better and how it will change after sleeve gastrectomy. You will also be described as the lead in a very low-calorie diet, usually for two weeks. This lead in diet is to allow some of your visceral fat stores (fatty liver and omentum) to reduce a little thereby allowing better access and views at your surgery and to achieve a superior surgery outcome. In the days leading up to surgery, the hospital will contact you and reiterate the preparation for the surgery. The patient will fast from midnight and be asked to turn up on the day of surgery.
The Surgical Process
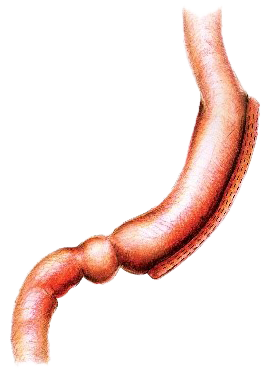
You will be seen by Dr Le Page again just before having the surgery. This is under general anaesthetic which means that you are fully asleep, and will not experience pain or awareness of the surgery at all. Dr Le Page then prepares for the surgery with his surgery assistant. In a sterile fashion four ‘keyholes’ are used to access the stomach and complete the surgery. The keyholes include three 5mm access ports (smaller than your phone’s charging port) and one 15mm in size, the latter being hidden in the belly button or umbilicus which produces a superior cosmetic outcome for you. The stomach is identified at surgery once the liver is lifted (this is the importance of having a pre-surgery liver shrinkage diet to make this more accessible for Dr Le Page and safer for you). With an advanced keyhole energy device, the attachments and blood vessels to the stomach are sealed and divided which then allows the stomach to sit freely ready for stapling. A tube (called a bougie) is passed down the mouth of the patient under anaesthetic. This tube allows Dr Le Page to calibrate the size of the sleeve gastrectomy thereby removing around 85% of the stomach and leaving a tube that holds between 100 to 150 millilitres. The tube also allows the shape of the tube sleeve stomach to be fashioned accurately by Dr Le Page so that the small food you will eat can pass throughout without getting blocked, which could cause discomfort or vomiting otherwise later on (the importance of this can sometimes be overlooked by surgeons).
Once the stapler has been passed next to the temporary bougie tube in the stomach it is sequentially fired to seal the new small stomach and divide it from the part that will be removed. Very small staples remain on the tube stomach which keep this sealed. The staple line created will need to heal and this becomes incorporated with scar tissue over time such that these staples are not even visible several months later. The stomach that is being removed is in a deflated state and this fits through the 15 mm keyhole port site at the Umbilicus/belly button so this does not need a large incision to remove. This part of the stomach is removed permanently and can never be returned. This however does not contain any essential components as the remaining tube stomach still secretes the stomach juices as part of normal digestion. Dr Le Page then inspects the internal organs and the sleeve stomach to ensure that it looks to be of an ideal shape and size and also that there is no sign of any bleeding. Some stitches or sutures are used at this time and also an assessment is made of the reflux valve above the stomach on the diaphragm. If the diaphragm here is slightly widened this allows a hiatus hernia to form so if there is a suggestion of this Dr Le Page will stitch this so that it is snug around the food pipe/oesophagus above this tubular sleeve stomach. If this is not done the sleeve stomach will tend to slide through the diaphragm as a hiatus hernia and lead to a heightened risk of reflux. After this surgery, the incision sites are stitched up with absorbable stitches which are buried beneath the skin and are not even seen. The bougie tube is removed before the patient wakes up.
Post-Surgery Care
Waterproof dressings are then placed on top of the skin which allows the patient to have a shower that night of surgery. The surgery itself will take about 45 minutes. You will wake up from the anaesthetic in the recovery room. Dr Le Page will call your nominated family or friend to update them after the surgery. You will move to the ward after about 1 hour in the recovery room and be attended to by the nurses.
With modern anaesthetics, Dr Le Page finds that when he reviews patients in the hours after surgery they usually describe minimal pain and usually just feel very tired due to the anaesthetic. It is also not common now to have significant nausea in the hours after surgery although this can persist until the evening and occasionally the next morning. With a modern medication regime, the nurses do keep an eye on these factors and can give additional medication as needed. The patient will be able to walk from the bed with the assistance of the nurses to the toilet and they are encouraged to move around the ward as they tolerate. This will be quite free the following day Sips of fluid can be commenced later in the day of surgery very slowly. After waking up the next morning these are continued and if these are tolerated and the patient has recovered well and feels safe they may be discharged home with the prescribed fluid diet, a short supply of oral pain medicine and sometimes some dissolvable nausea wafers. Multivitamins can be commenced in the ensuing days to ensure adequate nutrition and these are continued daily under the supervision of the dietitian.
As described to you leading up to the surgery, the recovery phase usually means only an overnight stay in the hospital and then continuing a liquid diet for two weeks as outlined by the dietitian. This liquid diet is sipped regularly for the patient to keep hydrated and it also contains adequate protein and other essential ingredients along with the multivitamins. The diet is then progressed to a pureed ‘baby food’ type diet for a further two weeks and then onto soft food. During these phases, it is usual for a patient to not feel hungry, and often people state they crave less. This slow progression of diet is required as the staple line on the tubular sleeve stomach needs to heal and it is important not to pressurise it with any food boluses.
Long-Term Success and Monitoring
Dr Le Page reviews the patient at the two-week mark in the clinic and does a full check-up. It is common for patients to report that their experience of the surgery and recovery has been less impactful than they had thought. There is usually already a good weight loss that has occurred. The diet will be progressed with the help of the dietitian in the ensuing weeks and what Dr Le Page describes to patients is that once they get onto a soft diet they are usually having a few mouthfuls before they feel full. For some patients, it takes some time to get used to the new diet whilst others find it more easy. It is very rare for a patient to vomit and if they do it is usually because they have had one mouthful too many and they then know their limit. Unlike the gastric band, there should be no ongoing vomiting or food getting caught.
It is encouraged from the two-week mark to walk as much as tolerated as this will not damage anything and assist with your recovery and getting back to a normal life. It is encouraged to have an increasing exercise programme from around four to six weeks after surgery. It is important especially early on to ensure that a patient remains hydrated by drinking adequate fluids and not overly exerting with sweat on a hot day. There will also be a plan for the dietitian to establish regular eating pattern with an increasingly broad range of healthy foods. It is quite common for a patient’s taste to change such that they avoid anything overly fatty or sweet. Many patients report less hunger which is usually explained by a reduction in the hunger hormone Ghrelin which is mostly produced by the part of the stomach removed during the surgery.
Dr Le Page then sees the patient at the 3-month mark and checks how the progress is. If necessary, additional appointments can be made. Occasionally a patient may experience heartburn acid reflux but the majority of patients do not get this. The medication can be prescribed in this instance and also avoiding overeating and avoiding precipitating foods is important. Dr Le Page arranges contact by the coaching team who provide an individual session for the patient to identify goals and aspirations and also there are group sessions to assist with habit change and support for patients. This ranges from past habits that have contributed to the weight and health problems over time to adapting to a new life afterwards and new eating habits.
Dr Phil Le Page will outline the usual patient experience which is the gradual increase of portions over the ensuing months such that by about six months after surgery around half a cup of food can be eaten and at 12 months usually around 1 cup. Every patient is different but it would be usual for a patient to lose most of their excess weight in the first six months and depending on a patient’s starting weight it is quite standard to lose in the order of three-quarters of your excess weight. Most importantly Dr Le Page explains to the patients that this weight loss is a healthy mode of losing weight which is substantial and gradual but not overly fast. It is also not achieved through vomiting or food intolerance but rather a significant reduction in portions and usually reduced hunger and cravings. You help yourself during this process by making sustainable changes to your lifestyle and exercise habits.
Your Journey Back to Health!
Dr Le Page will continue to monitor you over the ensuing two years and keep reminding importantly that the surgery has produced a noticeable structural effect and continue to do so, however the more the patient can alter their lifestyle and habits that were existing before surgery the more likely the patient will have a long-term sustained improvement in health and weight. At the ongoing follow-ups he will undertake a full check-up, blood tests are done to check that the nutrition is adequate and also a reminder that multivitamins are recommended to be taken long term. The sleeve gastrectomy does not alter the flow of food through the bowel, unlike the gastric bypass which redirects food from the stomach to a distant part of the bowel by detouring the proximal small bowel. If a patient takes adequate intake of micro and macronutrients it is not common to find significant nutritional deficiencies. It is recommended a yearly blood parameter check is done and also at certain times further tests such as bone mineral density be done for patients having undergone bariatric surgery. Your GP should be involved with your ongoing care. We wish you the best on “your journey back to health!”