Broadly, cancer occurs when a cell in the body loses the ability to control its growth such that it grows and divides to form new cells uncontrollably. Normally the cells in our body have rules and ‘scripts’ to follow that include keeping the growth rate of cells controlled. If these ‘scripts’ become ‘unreadable’ by the cell (such as through a mutation in DNA which can occur any time a cell divides to create another cell) then the cell can keep dividing and creating new cells in an uncontrolled way. This is why cancer causes a lump as it contains many more cells than normal (and they look different under a microscope). The uncontrolled growth also means there are now more chances for further mutations in the DNA scripts that control how a cell should behave. This can allow cancer to spread to other parts of the body from where it would usually be found.
FAQs
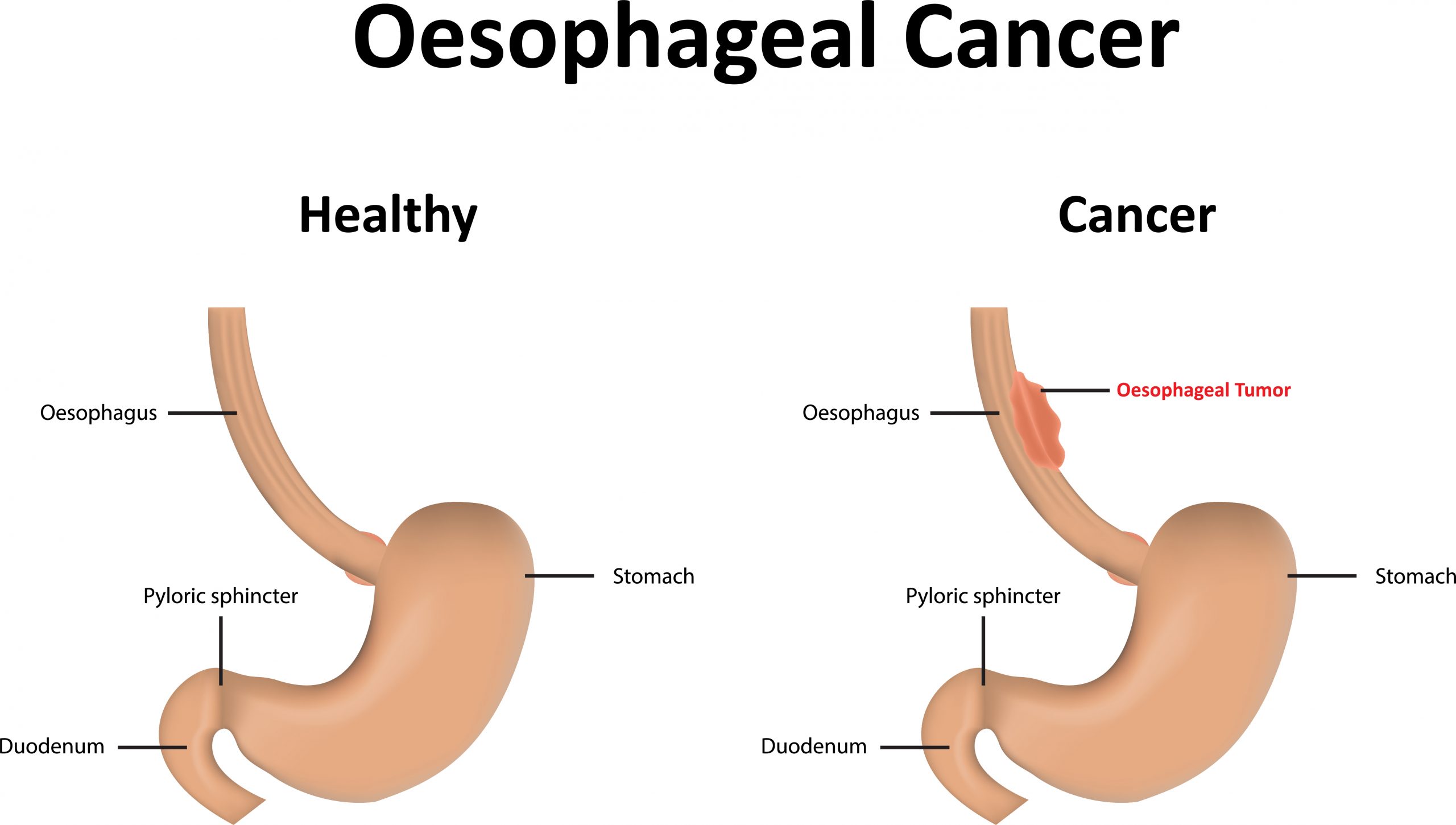
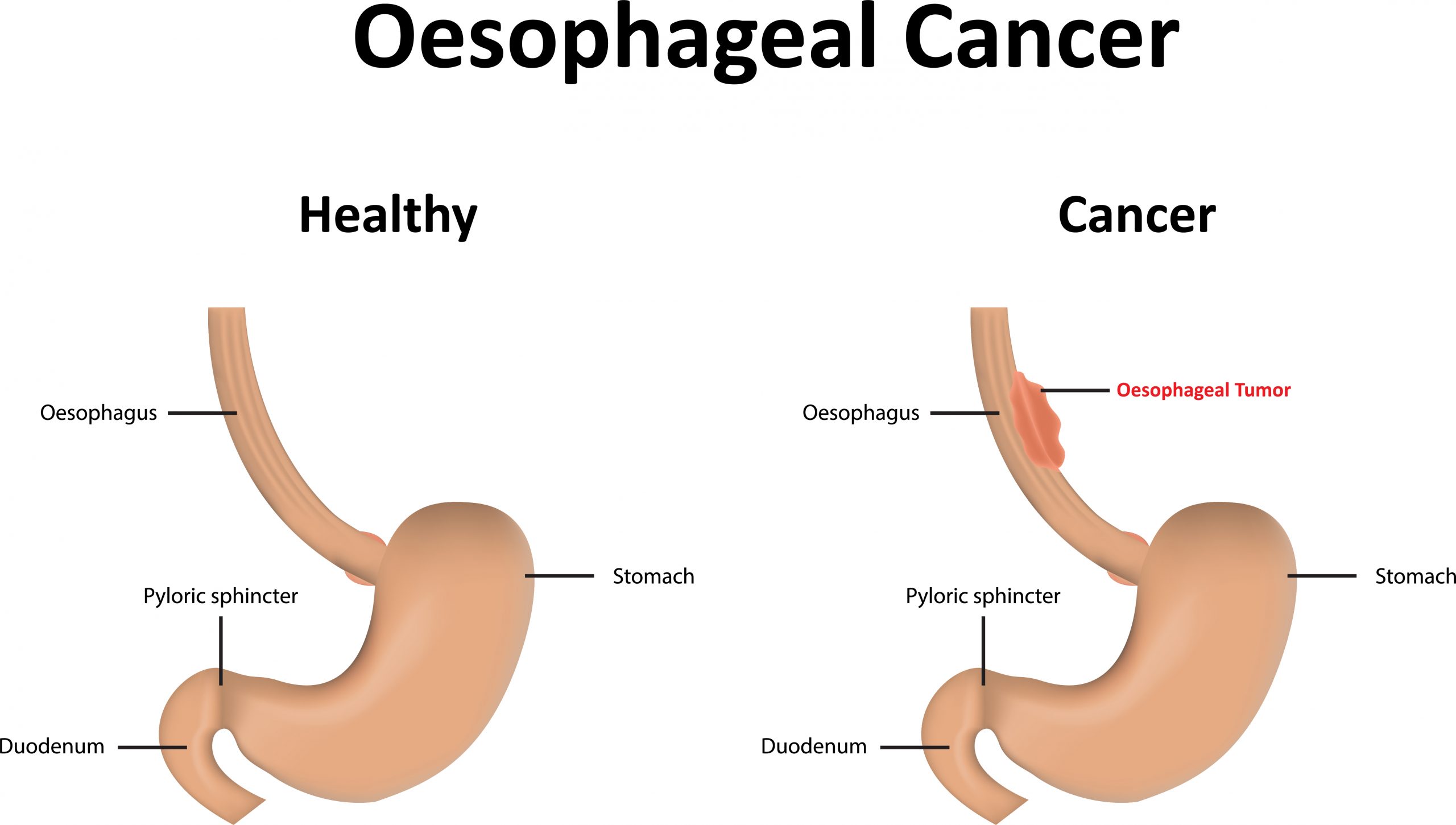
Why did I get oesophageal cancer?
At the fundamental level the cells lining the oesophagus have mutated and become uncontrolled in the way in which they divide to form new cells. This occurs at the DNA level inside a cell. The DNA may originally have had a propensity to mutate (such as when cancer ‘runs in families’) and/or suffer damage to them over time. In Western societies like in Australia the most common type of cancer is adenocarcinoma which can be caused by damage from Gastro-oesophageal reflux (GORD). It also has a higher association in males, caucasians and those who are overweight or obese. These may all be inter-related (such as when obesity leads to reflux which can cause oesophageal cancer), or it can just occur independently. In some people that develop this cancer there may not always be a significant history of reflux or other risk factor.
The other main type of oesophageal cancer that occurs is squamous cell carcinoma. It has a strong association with smoking. It is also the most common type in East Asia and it is thought to be due in part to high consumption of chemical carcinogens that can be present in certain foods like heavily smoked or pickled foods.
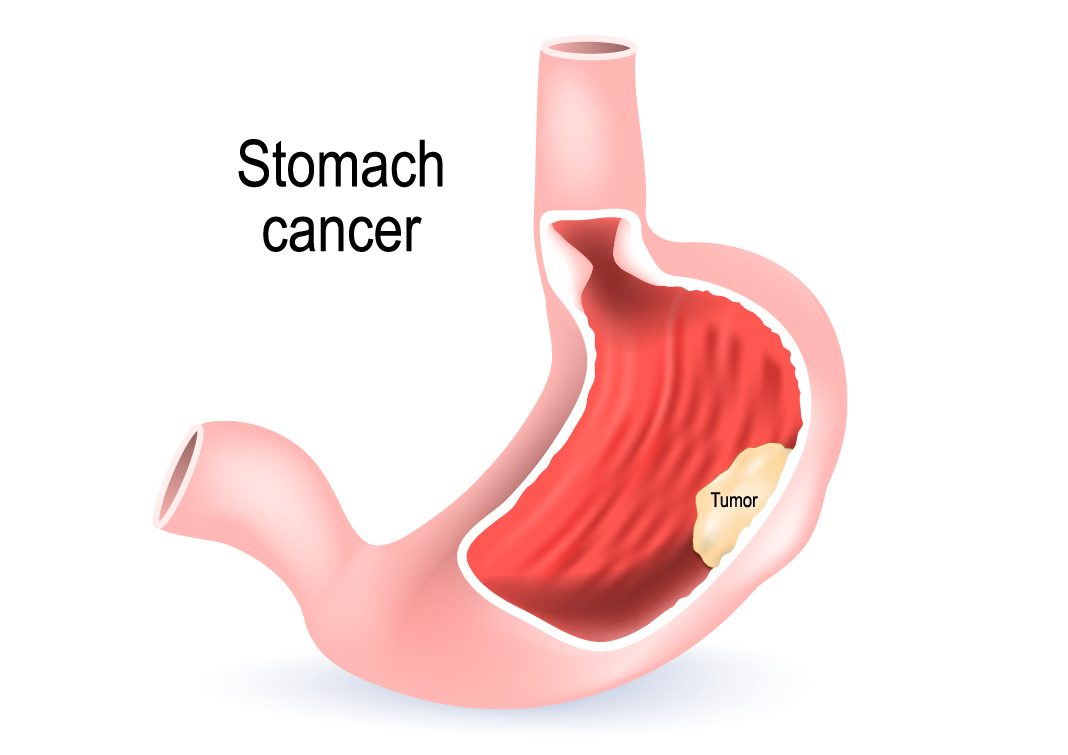
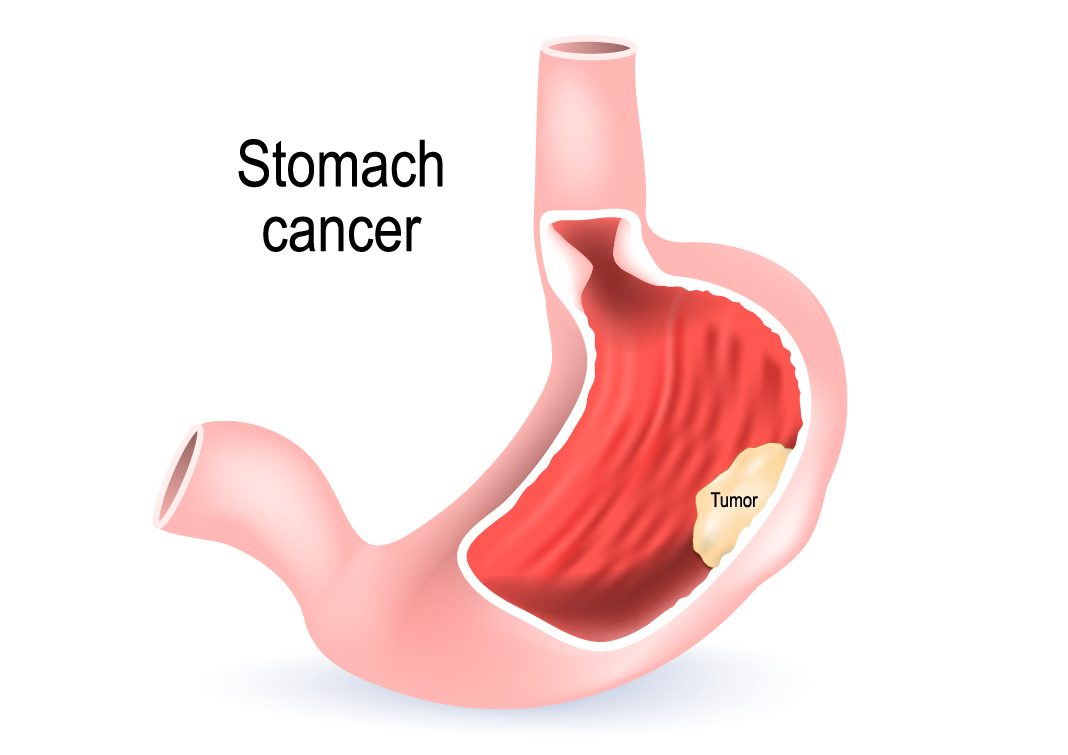
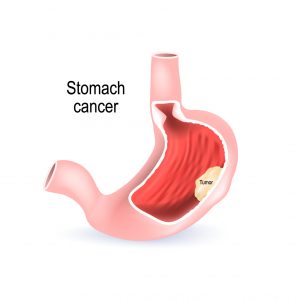
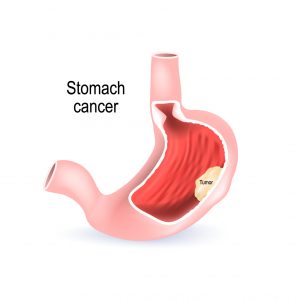
Why did I get stomach cancer?
The most common type of stomach cancer is adenocarcinoma and most often there will be no family history of stomach cancer, nor any other substantial risk factor. Other rarer types of stomach cancer include gastrointestinal stromal tumours (GIST) or lymphoma. In adenocarcinoma, at the fundamental level the cells lining the stomach have mutated and become uncontrolled in the way in which they divide to form new cells. This occurs at the DNA level inside a cell. The DNA may originally have had a propensity to mutate (such as when cancer ‘runs in families’) and/or suffer damage to them over time. In the lower part of the stomach it has a strong link to being caused by damage from the bacteria Helicobacter Pylori (H.Pylori), which also causes stomach ulcers. H.Pylori occurs more commonly in developing countries although it still occurs in Australia. People can have no symptoms or they may develop indigestion, pain in the top part of the belly or iron deficiency. In the top part of the stomach, stomach cancer is associated with being male, overweight, obesity and being Caucasian (note being associated with is not the same as being caused by).
Can I be cured of my Oesophageal or Stomach cancer?
The desired goal in treating patients with cancer is ‘cure’ of cancer. This approach is generally only feasible when the cancer has not spread to other organs or ‘invaded’ important structures next to it. The treatment approach most commonly consists of a combination of surgery, chemotherapy and sometimes radiotherapy. These are all done to ‘clear’ the tumour completely from being visible in the body or on x-ray scans. It is essentially never possible to provide a guarantee of cure, rather a calculation of risk of the cancer returning, which may range from being extremely unlikely to highly likely. Decisions about how to effectively treat the cancer involve a balanced decision of the chances of ‘cure’, risk of having surgery or chemotherapy or other risks to your health that may exist (eg. significant active heart disease or advanced age). These decisions are made by a number of cancer specialists that include your surgeon, gastroenterologist, oncologist, radiologist and pathologist at a multi-disciplinary meeting (MDT). The decisions and relevant issues should be conveyed to you by your specialist so you understand these important issues for you and you are involved with the decisions. After treatment you will continue to have follow-up to ensure there are no signs of the cancer coming back (“cancer recurrence”)
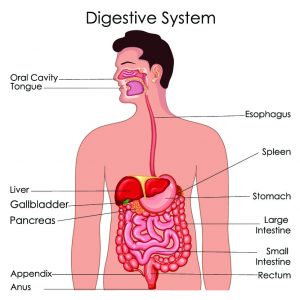
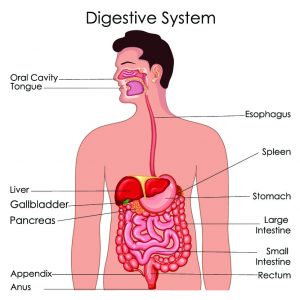
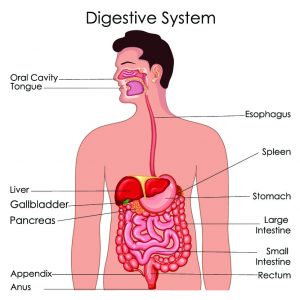
How can I eat if I need my stomach or oesophagus removed for gastric or oesophageal cancer?
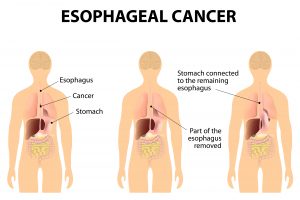
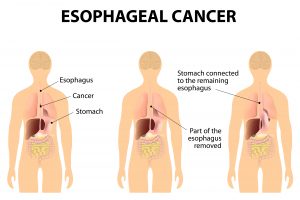
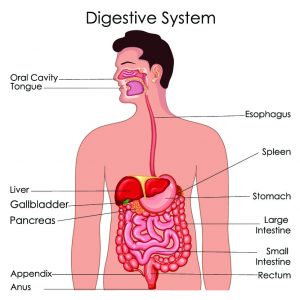
You will still be able to eat after uncomplicated surgery. The location of the cancer determines what part needs to be removed. Note the oesophagus is the food pipe which takes the food to the stomach which is an organ that can stretch to accomodate a large meal and allow digestion to occur. For stomach/gastric cancer, sometimes the surgery may remove only part of the stomach organ, less commonly the whole stomach is removed (and the oesophagus is then joined directly to the small bowel). For oesophagus cancer, usually only part of the oesophagus and stomach is removed and the remaining oesophagus is joined to the remaining part of the stomach. Given this, ‘continuity’ is maintained in the gastro-intestinal tract so swallowed food will still pass through your bowels. Meal sizes will be altered and digestion can be affected, however the expectation is that after recovery you will continue to be able to eat well and function normally.
How is surgery done for oesophagus cancer?
This is major surgery and should be done by surgeons skilled and experienced in managing patients with these cancers. This surgery is usually only performed with ‘curative intent’ such that the goal is to remove the whole visible cancer along with a margin of adjacent normal tissue along with lymph nodes (glands that drain fluid from where the cancer has been). It is often done after some chemotherapy +/- radiotherapy to improve the prognosis. The location of the cancer and the lymph nodes are identified allowing the surgical approach to be determined and how much oesophagus (and portion of stomach) needs to be removed. This may include an abdomen only approach (if near the junction of oesophagus and stomach) or both abdomen and chest approach (between the ribs for oesophageal cancer). The cancer is removed and the continuity of the gastro-intestinal tract is reconstructed, then all the surgery incisions are stitched closed. Laparoscopy/thoracoscopy or keyhole surgery is used when appropriate and safe to do so, otherwise open surgery is used to ensure the best change of complete cancer removal.
How is surgery done for stomach cancer?
This is major surgery and should be done by surgeons skilled and experienced in managing patients with these cancers. This surgery is usually only performed with ‘curative intent’ such that the goal is to remove the whole visible cancer along with a margin of adjacent normal tissue along with lymph nodes (glands that drain fluid from where the cancer has been). It is often done after some chemotherapy to improve the prognosis. The location of the cancer and the lymph nodes are identified allowing the surgical approach to be determined and how much stomach needs to be removed. This is often by laparoscopic keyhole surgery, although if it is advanced or large open surgery is sometimes used to ensure the best change of complete cancer removal. The cancer is removed and the continuity of the gastro-intestinal tract is reconstructed in a way that is best described in person at your consultation. All the surgery incisions are then closed.


What should I do now?
It is best to talk to your GP who will discuss with you about seeing an Upper Gastro-Intestinal Surgery specialist. You will need a referral from them to see Dr Le Page. You can choose a specialist of your choice in discussion with your GP. Dr Phil Le Page has been looking after such cancer patients and performing this surgery for the last 10 years. He is specialised in this field, has regular contact with other cancer specialists and welcomes you to attend for a consultation.