“Reflux”, or “gastro-oesophageal reflux disease” (GORD), is a common problem in our society. Hiatus hernia is also a common problem. Not all patients with reflux have a hiatus hernia. Similarly, not all patients with a hiatus hernia have reflux. A person may have symptoms or be diagnosed incidentally with either of these conditions when undergoing tests for other reasons, such as an endoscopy or a CT scan. Some patients may need or choose to undergo Hiatus Hernia Surgery called Laparoscopic hiatus hernia repair and/or fundoplication. Hiatus Hernia Surgery in Sydney is available for those seeking effective treatment. Surgical treatment of a hiatus hernia is similar to that for surgery for reflux.
Read below for common questions and to understand this better.
FAQs
What is Reflux, or acid reflux, or GORD?
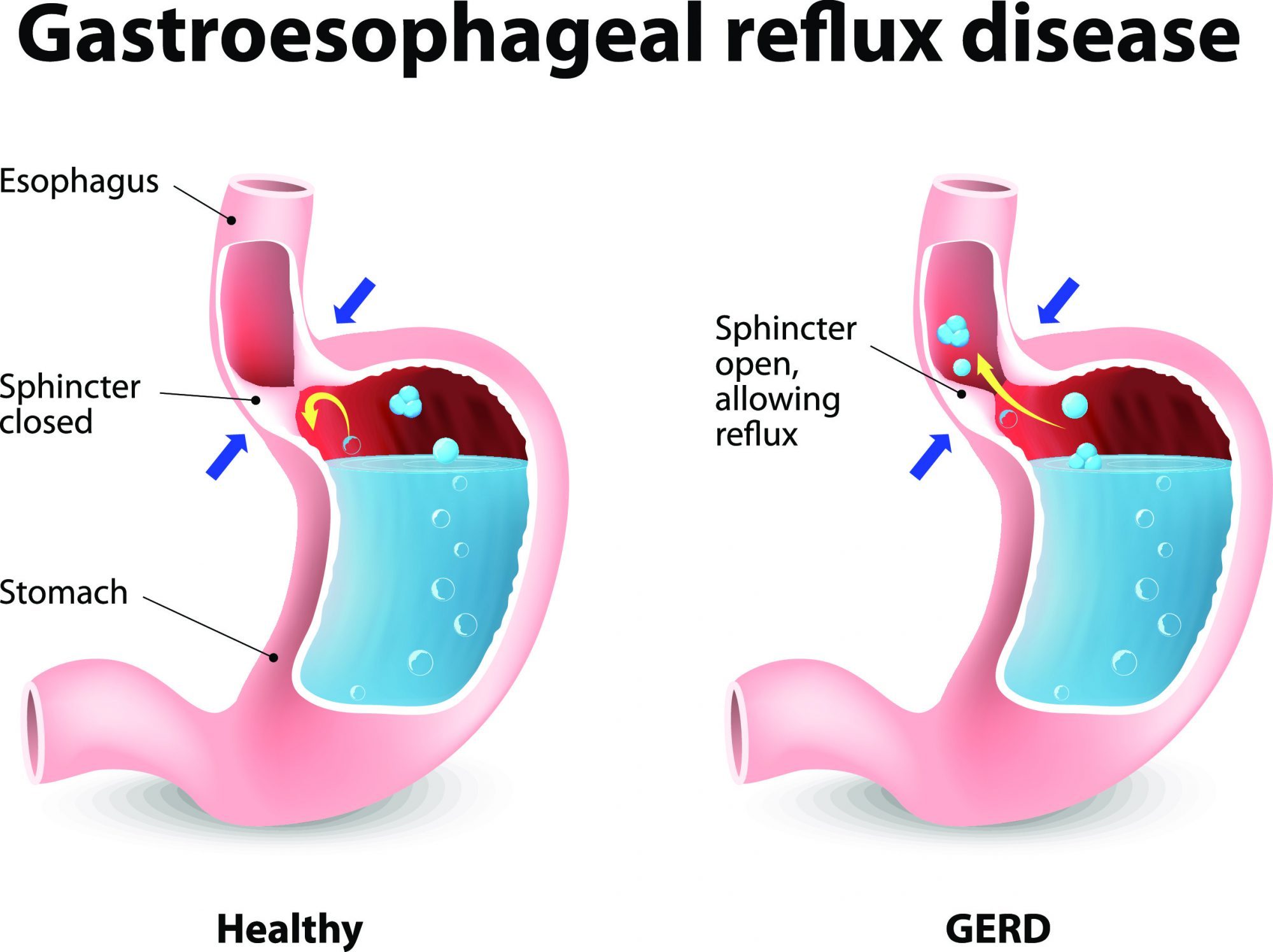
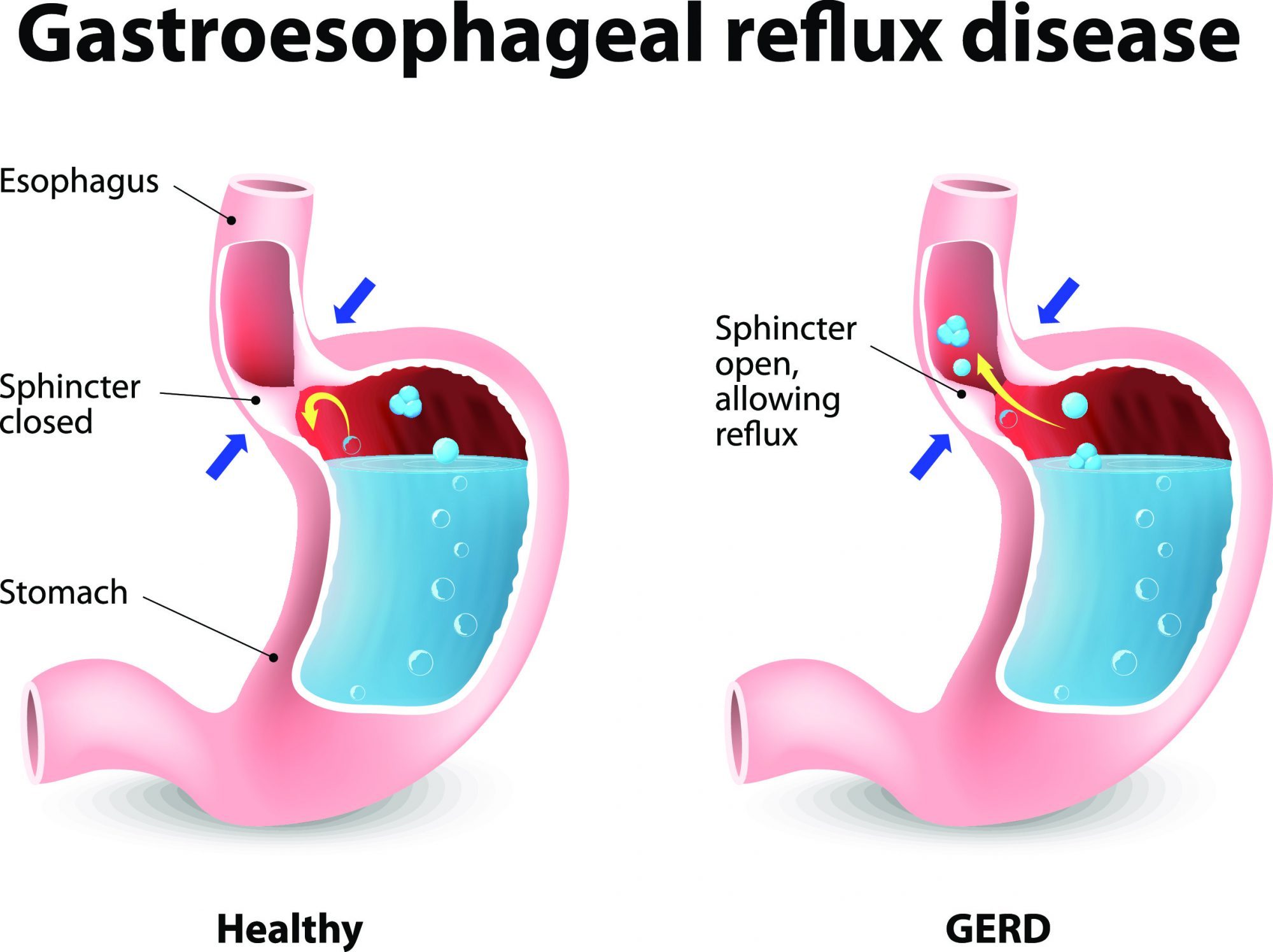
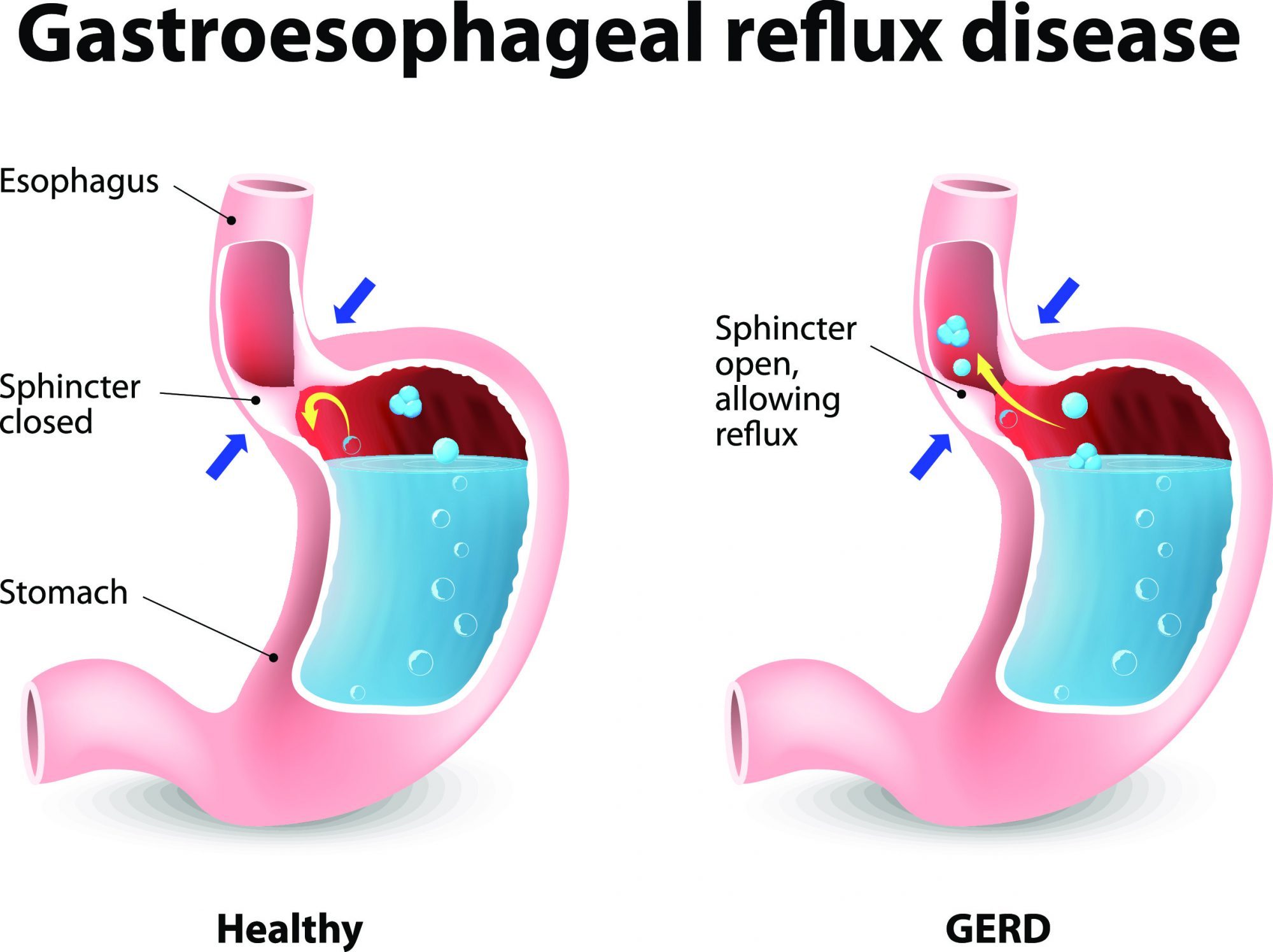
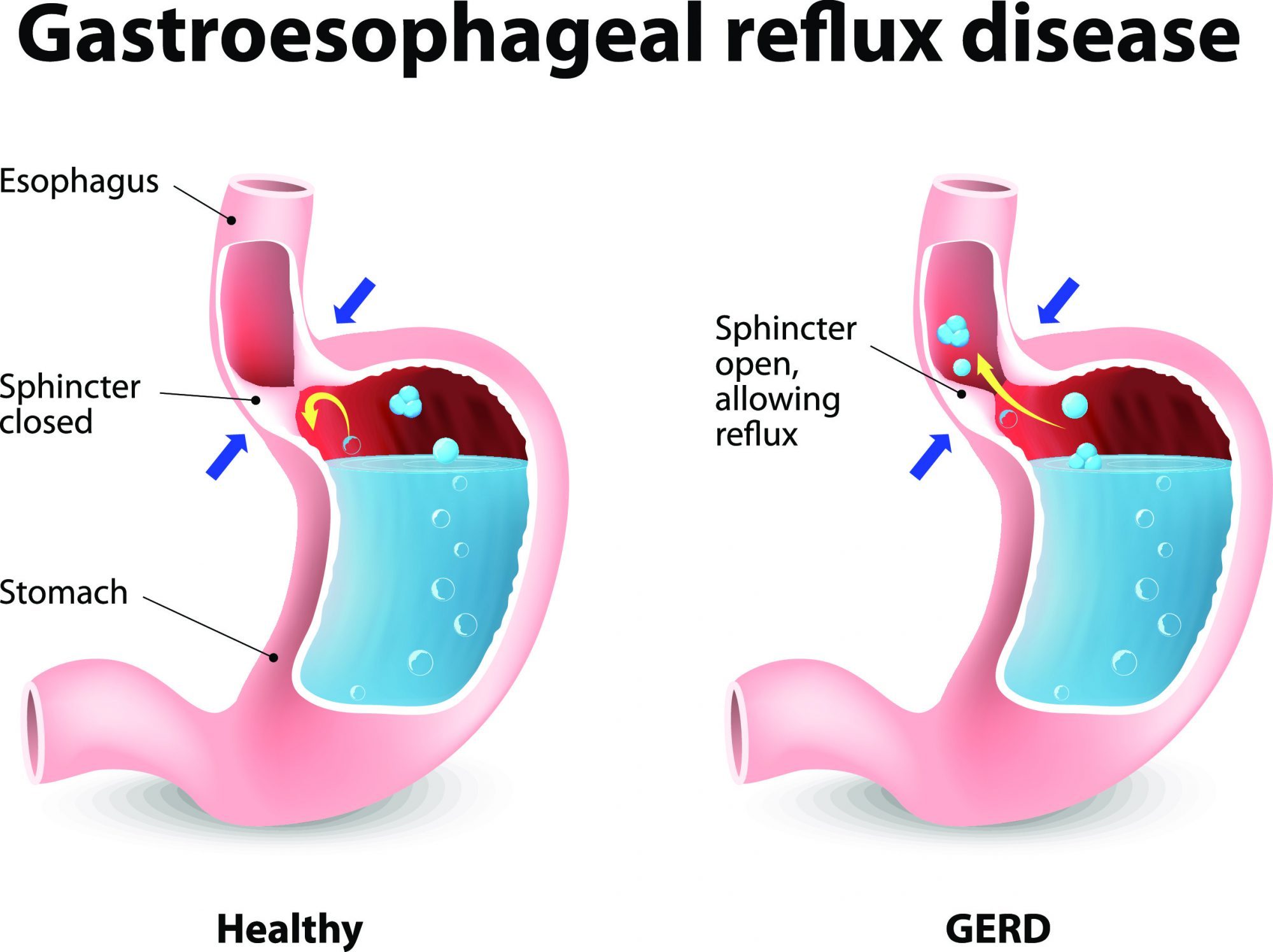
Water brash is a typical symptom of gastroesophageal reflux disease (GORD), it occurs when a person produces an excessive amount of saliva that mixes with stomach acids that have risen to the throat. A person experiencing water brash can get a sour taste in their mouth and would typically experience reflux as a feeling of “heartburn” or rising burning discomfort in the central chest.


This is because the contents of the stomach (which is normally in the abdomen or ‘belly’) are acidic, and this passes up out of the stomach into the oesophagus (‘gullet’ or ‘food pipe’) behind your breastbone, which will create the burning sensation. Occasional reflux is considered normal, but when it becomes excessive or problematic it is abnormal. Other feelings can be experienced too, such as a feeling of fullness or fluid rising to your throat, an ‘off’ taste in your mouth (known as ‘acid waterbrash’), excessive belching, cough, throat clearing or voice changes (‘laryngo-pharyngeal reflux’ or LPR). Occasionally, reflux can ‘silently’ pass into your lungs as aspiration causing a chest infection or cause shortness of breath. The reflux may be caused by a variety of things, such as certain foods or drinks, or by a weakness in the ‘valve’ between the stomach and oesophagus. A hiatus hernia, as described below, may contribute to this weakness of the valve, but not always. Remember, not all patients with reflux have a hiatus hernia. Similarly, not all patients with a hiatus hernia have reflux.
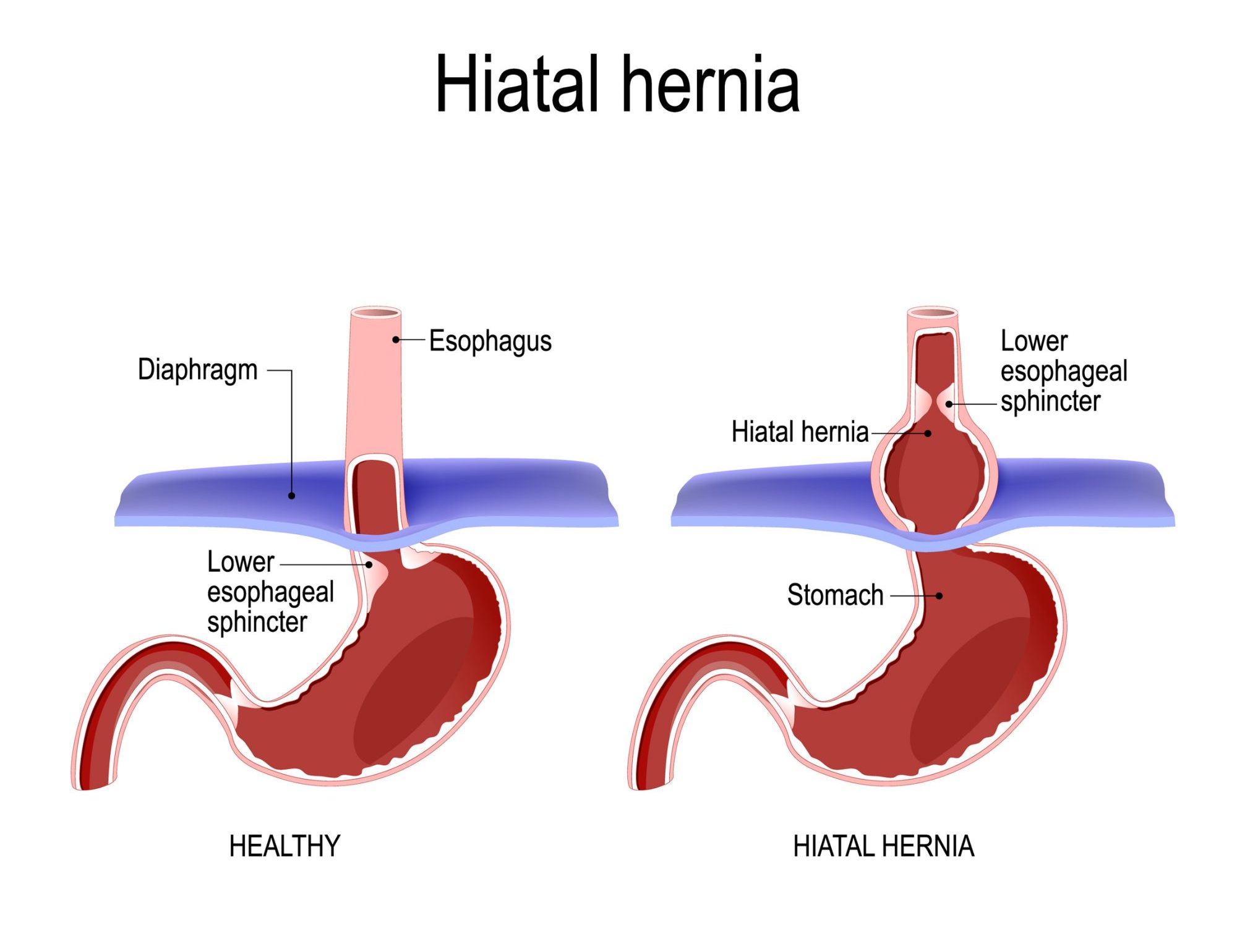
What is a hiatus hernia?
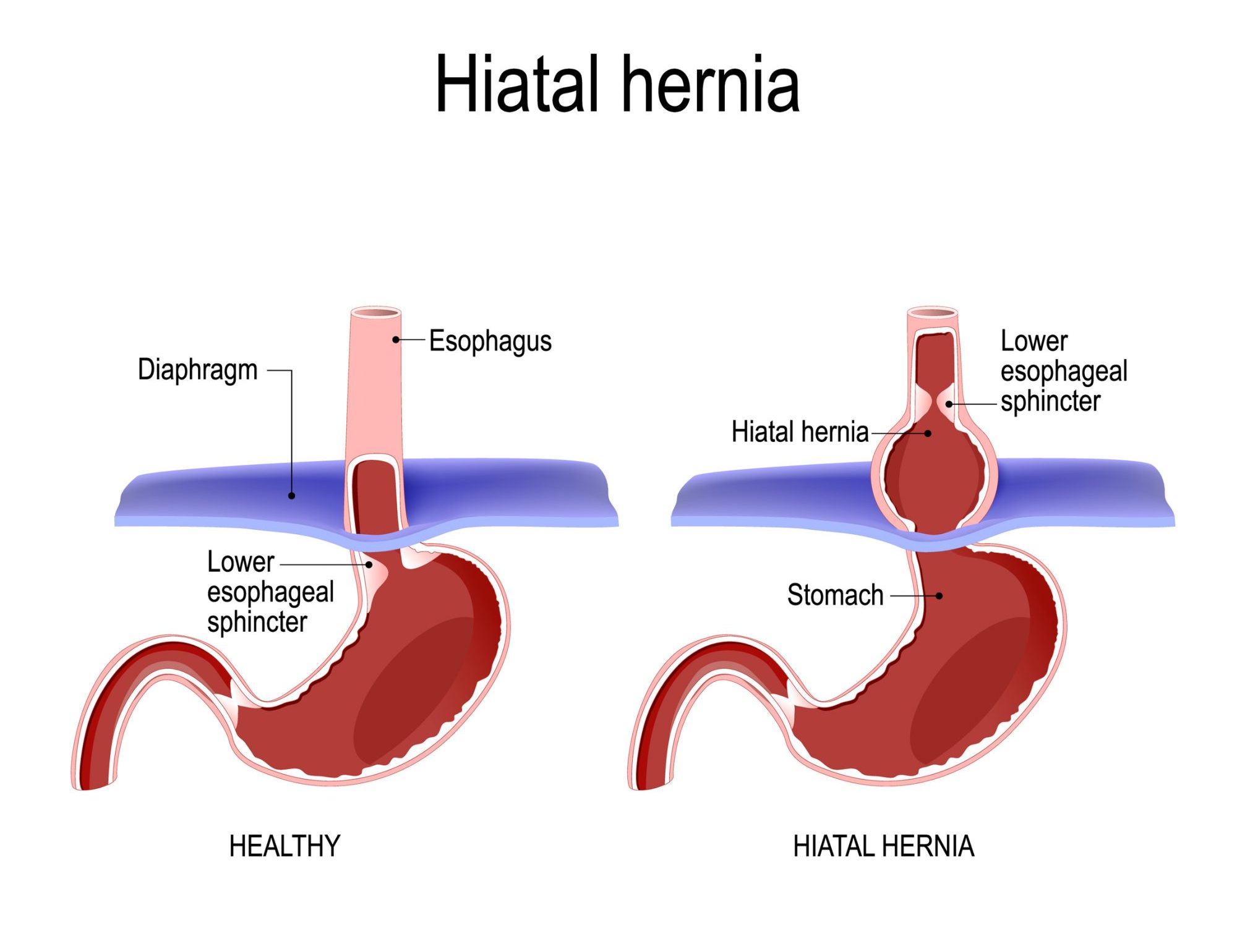
A hiatus hernia is where the gap in the diaphragm is abnormally wide (the gap allows your oesophagus/food pipe to pass from your chest into your belly). The diaphragm is the main breathing muscle and separates the abdomen cavity (‘belly’) from the chest cavity. Normally this gap is ‘snug’ around the oesophagus but a widened gap due to a hiatus hernia allows the stomach (or other abdominal organs) to pass through the wide gap into the chest cavity. This is abnormal. Small hiatus hernias are relatively common. Patients can sometimes be unaware of their presence.
Not all patients with reflux have a hiatus hernia. Similarly, not all patients with a hiatus hernia have reflux.
Is Reflux a serious problem?
If someone experiences reflux regularly this is normally quite uncomfortable. Depending on how frequent and bothersome this is for a person determines if treatment such as surgery should be performed. More serious consequences can occur. With long term inflammation from reflux (either acid or bile) oesophagitis and ulcers can form in the oesophagus. This can cause bleeding and scarring which could affect someone’s ability to swallow. Reflux can lead to development of Barrett’s Oesophagus which is a known precursor to oesophageal cancer (albeit rare). Additionally, it is thought that chronic inflammation from reflux (without Barrett’s) is the reason why oesophageal cancer is more common in patients with reflux (albeit still very rare).
What is Barrett’s Oesophagus?
This is where the type of lining on the inside of the oesophagus (mucosa) changes from its normal type of lining. This can be seen by the naked eye during an endoscopy and confirmed under microscope testing of biopsies of the area (showing the different type of mucosa lining). The importance of Barrett’s oesophagus is that there is a higher chance of developing oesophageal cancer (albeit still rare).
Should I take medication or have surgery for my reflux?
It is most important to address lifestyle reasons that may be contributing to reflux. These include avoiding foods that you know cause it (this may be spicy foods, or excessive alcohol or sometimes even more bland foods). Also avoid large meals which excessively distend the stomach. Eating shortly before going to bed leaves food digesting in your stomach when you lie flat, encouraging reflux to occur (if you still get reflux at night you could prop the head of your bed up). Being overweight or obese also causes reflux so losing weight should help.
Beyond these measures it is usually best at trailing medication for reflux in the first instance. This may be on an as needed basis and antacids (such as quickeze, gaviscon or mylanta) act quickly to neutralise the acid that causes heartburn. If more regular medication is necessary the most common medications are from a group called ‘proton pump inhibitors’ (such as nexium or somac). Another group is called ‘H2 blockers’ and includes Nizatidine. These medications reduce the acid that the stomach produces, however they do not stop the reflux itself as the valve at the stomach entrance remains weak.
Many patients have surgery for reflux and they must be selected appropriately and counselled well by their doctor. If heartburn persists despite addressing lifestyle factors and taking acid reducing medication then surgery should be considered. If a patient decides they do not wish to take medication long term (for reasons of potential side effects, medication cost or hassle) then surgery can be considered as an alternative.
If medication stops the burning sensation but still leaves the feeling of fluid or food particles rising up towards your throat then surgery is best (as medication cannot stop the presence of fluid or food nor the mechanical reasons for the reflux occur in the first place).
More significant reflux, such as where it travels up and ‘aspirates’ into your lung, would suggest a stronger reason to undergo surgery. As does the presence of a hiatus hernia which may be causing other problems in addition to reflux.
What problems does a hiatus hernia cause?
Small hiatus hernias are relatively common. Patients can sometimes be unaware of their presence. If they do cause problems it would usually be the sensation of “reflux”, as described above (read above for more information about reflux/GORD). This occurs as the diaphragm muscle no longer acts as a sphincter (or like a one way valve) to stop stomach contents rising into your chest. Because the hernia is a mechanical problem (the stomach has moved into the chest cavity), it can also cause unique problems, such as food getting stuck or caught leading to acute pain or vomiting. It may also cause a small ulcer where it rubs on the diaphragm which can cause bleeding or iron deficiency anaemia. Increasingly, evidence exists that the herniated stomach can compress the heart or lungs and cause shortness of breath. Occasionally, the worrying and potentially life threatening problem of the stomach twisting (‘volvulus’) can occur (and often there would be intermittent symptoms leading up to this). This is because in large hiatus hernias the stomach becomes very floppy and liable to twist (usually it is held in the abdomen by ligaments but when these ligaments stretch the whole stomach can move into your chest). This is a bit like a tent which is normally held tight by ropes to tent pegs in the ground – if the ropes stretch or loosen this may allow a wind to blow and kink and potentially twist the tent.


If there is a concern this is happening, this is a strong indication for surgical repair. Other organs can also occasionally pass into the chest, such as the bowel or spleen. Another type of hiatus hernia is a para-oesophageal hernia whereby part of the stomach separately comes up as a hernia next to the oesophagus. Because it is separate it can get trapped (incarcerated) and thereby causing discomfort, pain, trouble swallowing and gangrene (from lack of blood supply).
Do I need my hiatus hernia fixed?
This depends on what problems this is causing you and also a medical judgement on the risk of complications from the hernia. Strong indications to repair a hiatus hernia are a medical concern for a full volvulus of the stomach (twisting as described above), problematic reflux, compressive symptoms causing heart compression and shortness of breathness, and ulcers from hernia rubbing causing ongoing iron deficiency anaemia.
How is surgery performed for a hiatua hernia or reflux/GORD?
Tests that patients may need beforehand include gastroscopy (endoscopy), barium swallow (xray with swallowed dye), CT scan, and/or catheters passed down into the stomach to measure acid and assess the swallowing muscles.
Surgery to address problematic reflux and/or hiatus hernias is termed laparoscopic fundoplication or laparoscopic hiatus hernia repair. The fundoplication is where part of the stomach is wrapped around the lower oesophagus to help/reinforce the anti-reflux ‘valve’ (the valve would have been weakened over time). The hiatus hernia repair is done when a hiatus hernia is present, and requires repair of the wide diaphragm gap, and to free the stomach in the chest to allow it to be brought back to its normal position and stitched there. If the stomach is also twisted (volvulus), it is untwisted and straightened when it is brought down. These are keyhole operations that usually requires a 1-2 night hospital stay. The exact components which may make up your operation depend on these factors, in addition
to individual factors as discussed with your doctor. It is important you are assessed by a specialised surgeon trained in these techniques, to determine if or how and when an operation is required.


After surgery, you are usually in hospital for 1-2 nights and commence on oral liquids under observation. You will be able to mobilise on the day of surgery and will be encouraged to walk the following day to assist your recovery. After discharge follow the dietary instructions as outlined below. Reflux medication will usually be continued for a short time until review with your doctor. After a number of weeks the expectation would be that swallowing will become easier. You may feel food passes a little slower and you may fill up sooner, which should settle with time. A small degree of weight loss can occur during this time. A noticeable improvement of reflux should be noticed and depending on your situation reflux medication should be able to be stopped after review. The expectation is that a normal diet should be able to be taken, but occasionally certain foods like white bread or steak may be more difficult. Rarely an endoscopy may be needed later on to open up the valve slightly. Occasionally, “post-fundoplication” symptoms can occur which may include a feeling of abdominal bloat, increased passage of flatus, loose bowels or difficulty belching. All things considered, multiple research studies have shown high levels of satisfaction for patients undergoing the surgery.
As the healing occurs, the stomach further settles into position within the abdominal cavity through your body’s production of scar tissue. Given the tissues have been inherently weak which led to the hiatus hernia forming in the first place, there is a possibility the hiatus hernia can come back (research studies have shown this despite various techniques being tried to prevent this from occurring). Most times, however, this will not lead to problem symptoms. Rarely, would a re-operation be required.
What should I do now?
It is best to talk to your GP who will discuss with you about seeing an Upper Gastro-Intestinal Surgery specialist. You will need a referral from them to see Dr Le Page. You can choose a specialist of your choice in discussion with your GP. Dr Phil Le Page has performed hundred’s of Reflux and hiatus hernia operations and is specialised in this field and welcomes you to attend for a consultation.