What are the types of Weight Loss Surgery and are they permanent?
- There are 3 main options for your surgery which will be discussed in your consultation. All are done by keyhole surgery (laparoscopy) and usually have a 1-2 night hospital stay. Usually the favoured option is the Laparoscopic sleeve gastrectomy but other options may be more appropriate for your unique situation. The sleeve gastrectomy makes permanent changes to your stomach by removing a large expandable portion of your stomach to restrict your intake and make you feel less hungry. The Gastric bypass and Gastric band are reversible by undergoing further surgery if this ever became necessary (although scarring changes on the stomach will remain).
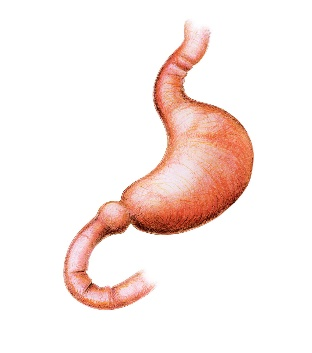
- In the normal stomach, food swallowed passes down your oesophagus (food pipe or gullet) and enters the stomach (after passing through a ‘gap’ in the diaphragm called the “hiatus”). Food is held in the stomach for digestion (to break it into small particles). The stomach can stretch to hold a large meal. Gradually these small particles are pushed through the valve (“pylorus”) at the lower end of the stomach to enter the duodenum which is the first part of the small bowel. The nutrients (and calories) in food are absorbed in the small bowel (of which there is usually around 6m). It then passes into the large bowel before being excreted as faeces.
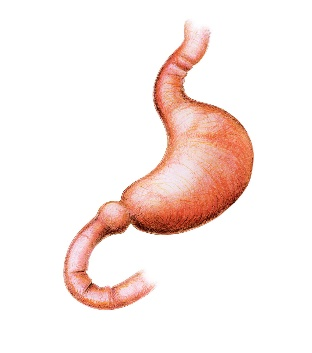
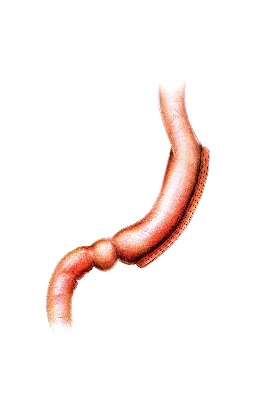
- After the Laparoscopic Sleeve Gastrectomy the stomach volume is markedly reduced, significantly lowering your meal sizes, and the ‘hunger hormone’ ghrelin level drops in the blood which usually means a person will have a reduced desire to eat. This is the most commonly performed obesity surgery operation in Australia. It has a high success rate at achieving extensive weight loss (mainly in the first 6-9 months) and allows for a good eating quality. It is a safe procedure and there is no re-plumbing or shortening of the bowel. Food is still absorbed in the normal way.
- After the Laparoscopic gastric bypass, the stomach size is dramatically reduced and the bowels are “re-plumbed” to bypass the first part of the small bowel. Two types of bypass exist.
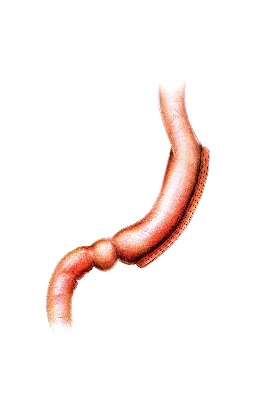
- The “mini” gastric bypass (or “omega loop”, “single anastomosis”) sees the bowel joined onto the small stomach pouch (usually bypassing 1.5-2 metres of bowel)
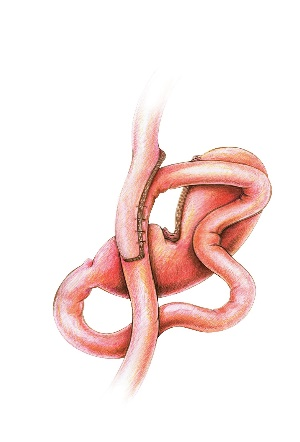
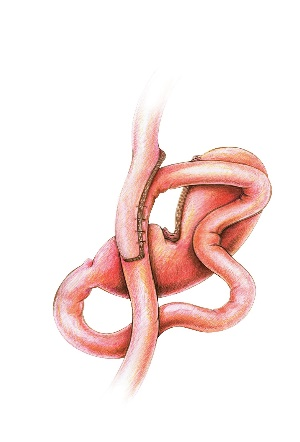
- The Roux-en-y gastric bypass sees the small bowel joined onto the small stomach pouch but also to itself lower down to make the bile inside the bowel flow away from the stomach pouch.
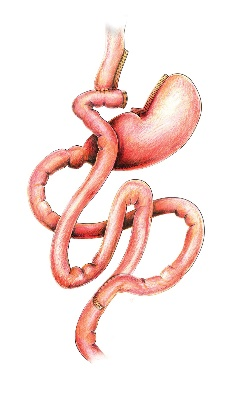
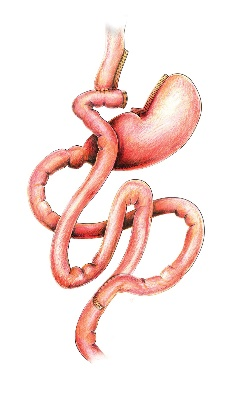
- Both laparoscopic gastric bypass are powerful operations for weight loss and metabolic health improvement. It has been performed for many decades and the excellent results have stood the test of time. Technical advances more recently have made it a safe and well tolerated procedure when performed by a specialist surgeon. It works by a number of strong mechanisms, including creating very small meal portions and significant alteration to hunger and appetite hormones. It is the most effective operation to reverse diabetes (often seeing patients come off their medication altogether early after surgery). There is an alteration to the food stream within the bowels (leading to metabolic improvement) which means it is critical to maintain follow-up with a team specialised in managing and monitoring patients after surgery.
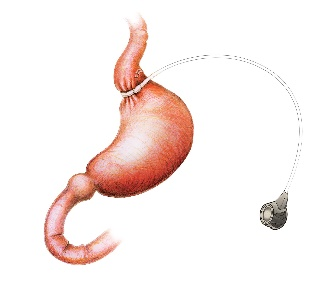
- After the Laparoscopic gastric band a soft plastic ring around the top part of the stomach (effectively separating the small part of the stomach above the band from the large stomach volume below the band). The ring size is adjusted during follow-up by inflating or deflating this ring, done by accessing a ‘port’ which sits within the abdominal wall (hidden under the skin). Portion sizes are thereby reduced and often hunger is suppressed (by the band pressing on the hunger nerves in the stomach). The laparoscopic adjustable gastric band (LAGB) has been a commonly performed procedure since the 1990’s to help patients achieve significant weight loss. It requires a commitment to eating in appropriate ways for the band to be effective and the appropriateness of this procedure for you needs to be discussed with your surgeon